A Vital Yet Overlooked Organ
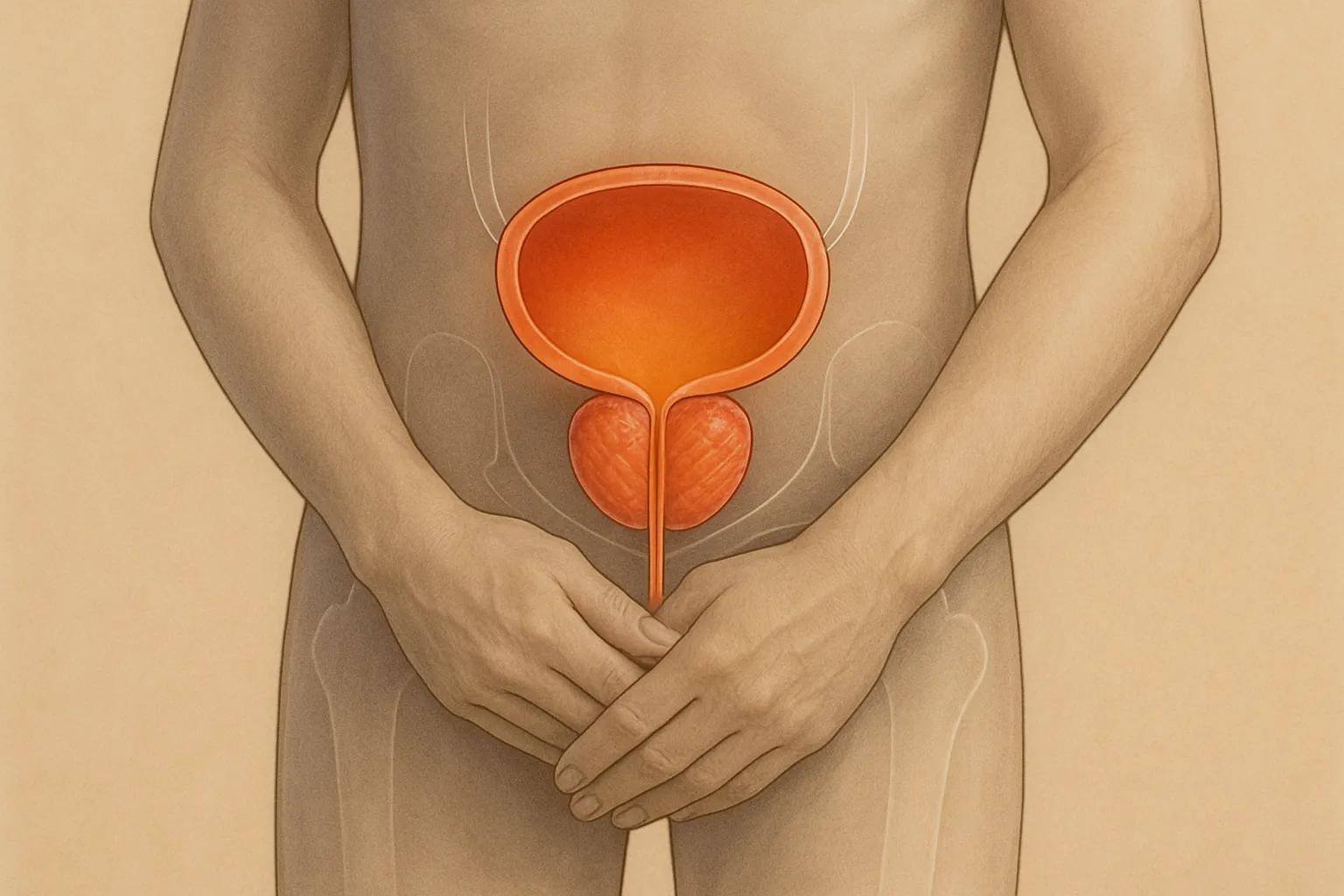
The prostate is a small gland that plays a big role in every man’s life, yet it often doesn’t get the attention it deserves. Located just below the bladder and in front of the rectum, the prostate surrounds part of the urethra and is responsible for producing fluid that nourishes and protects sperm.
For most men, the prostate functions silently and without issue—until it doesn’t. As men age, the likelihood of experiencing prostate-related problems rises significantly. In fact, most men over 50 will face at least one prostate issue in their lifetime, whether it’s enlargement, inflammation, or even cancer.
That’s why prostate health should never be ignored. Understanding how the prostate works, what conditions to watch out for, and how to take preventive action is essential for every man—regardless of age.
How the Prostate Changes With Age
Like many parts of the body, the prostate undergoes changes over time. Around the age of 40, it begins to grow—sometimes gradually, sometimes more rapidly. This natural enlargement is called benign prostatic hyperplasia (BPH), and while it’s not cancerous, it can cause uncomfortable symptoms that interfere with daily life.
In addition to BPH, men may develop prostatitis, an inflammation of the prostate that can be caused by infection or other unknown factors. And then there’s prostate cancer, one of the most common types of cancer among men, especially those over 50.
Although these conditions can be serious, many are treatable—especially when caught early. This is why awareness and regular monitoring are key.
Common Prostate Conditions Men Should Know About
1. Benign Prostatic Hyperplasia (BPH)
BPH is the most common prostate issue among aging men. It involves the non-cancerous enlargement of the prostate, which can press against the urethra and make urination difficult.
Typical symptoms include:
- Difficulty starting urination
- A weak or interrupted urine stream
- Frequent urination, especially at night
- A feeling that the bladder isn’t fully emptied
- Sudden or urgent need to urinate
Though BPH is not life-threatening, it can affect quality of life. Left untreated, it may lead to urinary tract infections, bladder stones, or kidney damage.
2. Prostatitis
Prostatitis refers to inflammation or infection of the prostate. It can affect men of all ages but is more common in younger and middle-aged men.
Symptoms may include:
- Pain or burning during urination
- Pelvic or lower back pain
- Painful ejaculation
- Frequent urination
- Flu-like symptoms (in acute cases)
There are several types of prostatitis, ranging from bacterial infections to chronic pelvic pain syndromes. Treatment depends on the cause and may include antibiotics, anti-inflammatory medication, and lifestyle changes.
3. Prostate Cancer
Prostate cancer is the second most common cancer in men worldwide. The risk increases with age, especially after 50. Although many forms of prostate cancer are slow-growing, others can be aggressive and life-threatening.
Risk factors include:
- Age over 50
- Family history of prostate or breast cancer
- African or Caribbean ancestry
- Obesity or poor lifestyle habits
Early-stage prostate cancer often has no symptoms. That’s why screening plays such an important role in detection and treatment success.
The Importance of Regular Screening
Many prostate conditions develop without clear symptoms. Fortunately, modern screening methods can help detect issues early—when treatment is most effective.
Two of the most commonly used screening tools include:
- PSA Test (Prostate-Specific Antigen): This blood test measures the level of PSA, a protein produced by the prostate. Elevated levels may indicate an issue such as BPH, prostatitis, or cancer.
- Digital Rectal Exam (DRE): A doctor feels the prostate through the rectal wall to check for size, texture, and irregularities.
Neither test alone is perfect, but together they provide useful insight. Your doctor will help interpret results and recommend further testing if needed.
When to Get Screened
- Age 50: Men at average risk should begin screening discussions.
- Age 45: Men with higher risk (family history or African ancestry) should consider starting earlier.
- Age 40: Men with more than one first-degree relative who had prostate cancer at an early age may benefit from even earlier screening.
Screening doesn’t automatically mean treatment—it means having information and being able to make informed decisions.
Supporting Prostate Health Through Lifestyle
While genetics and aging play a role in prostate health, your daily habits matter too. What you eat, how much you move, and how you manage stress all influence the condition of your prostate.
3. Diet and Nutrition
A balanced, anti-inflammatory diet is one of the most powerful ways to support prostate health.
Best foods to include:
- Tomatoes: Rich in lycopene, an antioxidant linked to reduced prostate cancer risk.
- Cruciferous vegetables: Broccoli, cauliflower, and cabbage help detoxify the body.
- Fatty fish: Salmon and sardines contain omega-3s that lower inflammation.
- Green tea: Packed with antioxidants that may slow prostate cell growth.
- Pumpkin seeds: A natural source of zinc, important for hormonal balance.
Foods to limit or avoid:
- Processed meats
- Fried and fast foods
- Excessive dairy and saturated fats
- Sugary beverages and snacks
4. Exercise
Physical activity helps control weight, reduce inflammation, and improve hormone levels—all beneficial for prostate health. Aim for at least 30 minutes of moderate-intensity activity five days a week.
5. Hydration and Urinary Habits
Drink plenty of water throughout the day, but limit fluids two hours before bed if nighttime urination is a problem. Avoid excessive caffeine and alcohol, which can irritate the bladder and worsen urinary symptoms.
6. Stress Management
Chronic stress may increase inflammation and impact hormone regulation. Meditation, deep breathing, hobbies, time outdoors, and regular sleep all contribute to emotional and hormonal balance.
When to See a Doctor
While annual checkups are vital, you should also speak to a doctor if you experience:
- Changes in urination patterns
- Painful urination or ejaculation
- Blood in urine or semen
- Erectile dysfunction
- Unexplained pelvic pain
These symptoms could signal a variety of conditions, including infections or cancer. Early diagnosis leads to better treatment options and peace of mind.
Treatment Options for Common Prostate Conditions
When it comes to prostate health, early detection is only half the battle. Understanding the available treatment options empowers men to make informed, confident choices if problems arise. While treatment depends on the specific condition and its severity, many options today are minimally invasive and highly effective.
Treating BPH (Benign Prostatic Hyperplasia)
For men with moderate to severe urinary symptoms due to prostate enlargement, several interventions are available:
1. Lifestyle and Behavioral Adjustments
- Reduce caffeine and alcohol
- Limit fluid intake in the evening
- Double voiding (urinating twice, a few minutes apart)
- Regular physical activity
2. Medications
- Alpha-blockers (e.g., tamsulosin) relax prostate and bladder muscles to improve urine flow.
- 5-alpha-reductase inhibitors (e.g., finasteride) shrink the prostate over time.
- Combination therapy is common and often effective.
3. Minimally Invasive Procedures
- UroLift: Small implants are placed to lift and hold enlarged prostate tissue away from the urethra.
- Rezūm Therapy: Uses water vapor to reduce excess prostate tissue.
- Laser Therapy: Removes excess tissue with precise targeting and minimal bleeding.
4. Surgery
- TURP (Transurethral Resection of the Prostate): A well-established surgical option that removes part of the prostate to relieve symptoms.
Your doctor will help assess which treatment best matches your symptoms, age, and overall health goals.
Treating Prostatitis
Prostatitis may come on suddenly or persist over time. Treatment depends on the cause:
- Bacterial Prostatitis: Usually treated with antibiotics, often for 4–6 weeks.
- Chronic Prostatitis/Chronic Pelvic Pain Syndrome: May involve anti-inflammatory medication, pelvic floor therapy, warm baths, stress management, and lifestyle changes.
Recovery can be gradual, so patience and consistent care are essential.
Treating Prostate Cancer
If cancer is diagnosed, treatment depends on its stage, aggressiveness, and your overall health. Options include:
1. Active Surveillance
- Ideal for slow-growing cancers
- Involves regular PSA testing, imaging, and biopsies
- May delay or avoid treatment for years
2. Surgery
- Radical Prostatectomy: Removes the prostate and surrounding tissue
- Often recommended for younger, healthy men with localized cancer
3. Radiation Therapy
- External beam or internal (brachytherapy)
- Suitable for localized or advanced cases
4. Hormone Therapy
- Lowers testosterone to slow cancer growth
- Often combined with radiation for aggressive cancers
5. Advanced Therapies
- Immunotherapy or targeted therapy for metastatic cases
The key to successful treatment is early detection, open communication with specialists, and thoughtful consideration of side effects, especially concerning urinary and sexual function.
The Emotional Impact of Prostate Conditions
Dealing with prostate health isn’t just a physical journey—it’s an emotional one. Men may feel embarrassed, isolated, or anxious about symptoms that affect their confidence, identity, or relationships.
It’s normal to experience a mix of emotions when facing issues like urinary difficulty, erectile dysfunction, or a cancer diagnosis. Left unaddressed, these feelings can lead to depression, low self-esteem, or withdrawal from partners and social life.
How to Cope:
- Talk about it: Speaking openly with your doctor, partner, or therapist helps reduce anxiety and build a support system.
- Join a support group: Many men find comfort and insight by connecting with others facing similar health journeys.
- Stay active: Physical movement boosts mood and reduces stress.
- Set realistic expectations: Some symptoms or side effects are manageable with time, treatment, and patience.
Mental health and prostate health are closely linked. Taking care of one supports the other.
Talking to Your Partner About Prostate Health
Conversations about prostate issues—especially those affecting intimacy—can feel uncomfortable. But honest communication builds trust, reduces shame, and invites support.
Here’s how to approach it:
- Choose the right time: Find a quiet moment when you’re both relaxed.
- Be direct but gentle: “I’ve been experiencing some changes I want to talk to you about.”
- Focus on connection: Remind your partner that this is about staying healthy and being present for each other.
- Invite support: Let them know how they can help—whether that’s coming to appointments or simply listening.
Partners often appreciate being included and want to help. Silence only creates distance—honesty builds closeness.
Prostate Health and Sexual Wellness
One of the biggest concerns men have about prostate treatment is its effect on sexual performance. While some treatments can affect libido or erectile function, many men continue to enjoy fulfilling sex lives with the right care and communication.
What to know:
- BPH and prostatitis may temporarily impact performance, but often improve with treatment.
- Prostate cancer treatments can cause temporary or long-term changes in erection or ejaculation, depending on the type of treatment.
- Recovery is possible: Pelvic floor exercises, medications (like sildenafil), counseling, and open communication with your partner all support sexual wellness.
Don’t be afraid to bring up sexual side effects with your doctor. Solutions exist, but they start with a conversation.
Long-Term Prostate Health Habits
Prevention and maintenance go hand in hand. Whether you’re symptom-free or managing a condition, daily habits matter more than you might think.
Top long-term strategies:
- Get regular checkups: Don’t skip annual physicals. Early detection saves lives.
- Eat a prostate-friendly diet: Include tomatoes, cruciferous vegetables, nuts, and healthy fats.
- Move regularly: Exercise supports hormonal balance and reduces inflammation.
- Manage stress: Chronic tension can worsen symptoms and harm immune function.
- Hydrate smartly: Drink plenty of water, but limit fluids close to bedtime if frequent urination is an issue.
- Know your numbers: Track PSA levels, cholesterol, blood pressure, and weight over time.
- Speak up: Don’t ignore symptoms or accept discomfort as “just aging.”
Consistency is more important than intensity. Small, daily actions add up to long-term benefits.
Breaking the Stigma: Prostate Health Is Normal Health
The biggest barrier to prostate care isn’t the symptoms—it’s silence. Men are often taught to “tough it out” or avoid discussing sensitive topics. But this outdated mindset leads to delayed care, unnecessary suffering, and avoidable complications.
Talking about your prostate isn’t awkward—it’s responsible. It’s a sign of maturity, self-awareness, and leadership. And when men lead by example, it encourages others to do the same.
Prostate health isn’t just a medical issue—it’s a quality of life issue. It affects how you sleep, how you connect, how you perform, and how you age. So speak up. Get screened. Stay active. And take control of your health, one step at a time.
Final Word
Every man deserves to understand his body—and his prostate is no exception. Whether you’re in your 30s, 50s, or beyond, proactive attention to your prostate can help you live longer, love better, and feel more confident in your everyday life.
Knowledge is power. Awareness is prevention. And action is what makes the difference.
Don’t wait for symptoms. Start the conversation. Ask the questions. Book the checkup. Because nothing is more masculine than taking care of yourself.