Why Prostate Health Deserves Attention
For many men, prostate health is rarely discussed—until something goes wrong. It’s one of those topics that’s often avoided out of discomfort, lack of knowledge, or the belief that it’s only relevant in old age. But the truth is, prostate health is something every man should start thinking about well before problems begin.
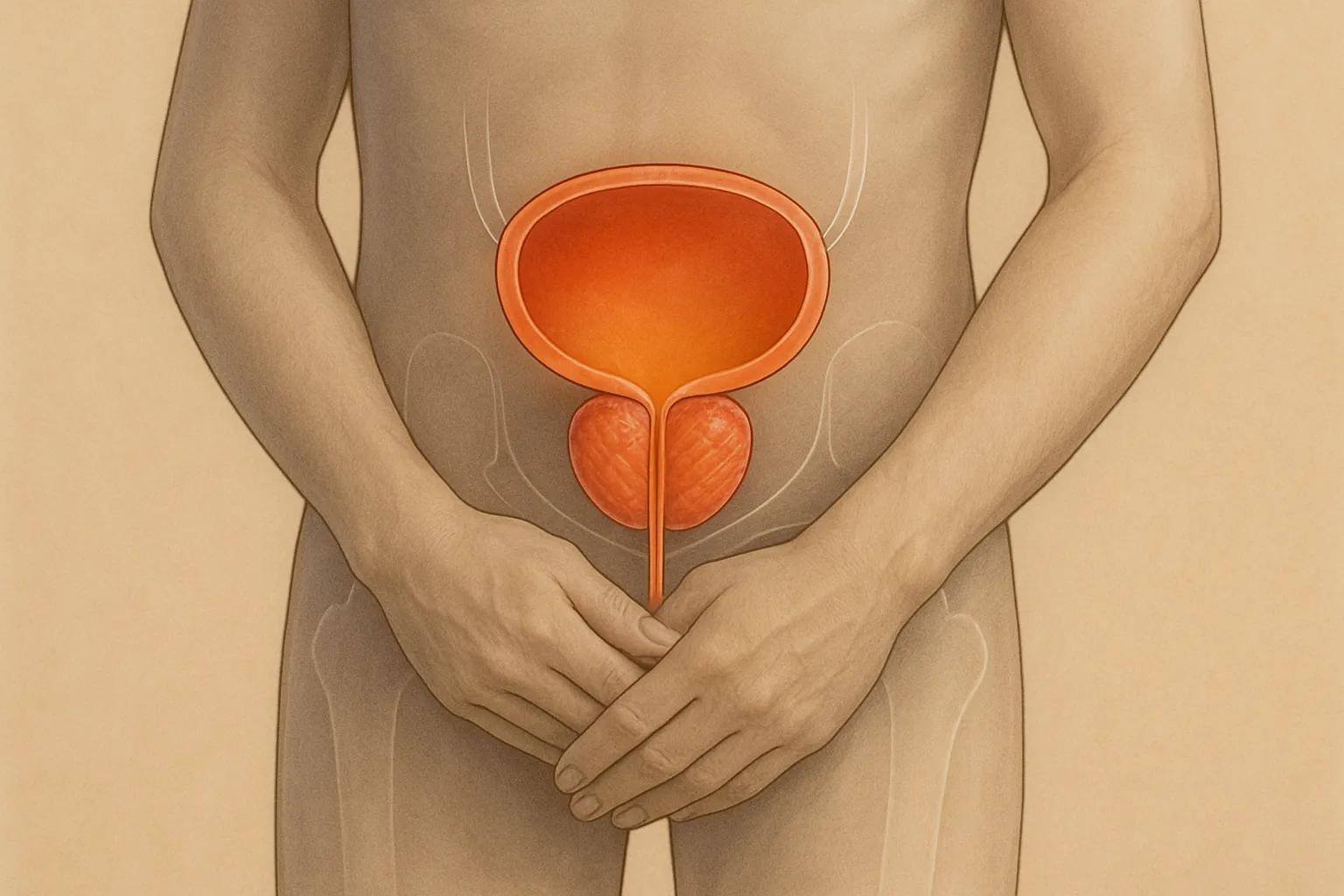
The prostate is a small gland, roughly the size of a walnut, located just below the bladder. It plays a key role in the male reproductive system by producing seminal fluid, which nourishes and transports sperm. Though small, its impact on health is significant—especially as men age.
After the age of 40, the prostate begins to change. For some men, this results in an enlarged prostate (benign prostatic hyperplasia or BPH), while for others, it can increase the risk of inflammation (prostatitis) or prostate cancer, which is one of the most common cancers in men.
The good news is that early awareness, regular screening, and lifestyle adjustments can significantly improve prostate health and reduce the risk of serious complications later in life.
Understanding the Most Common Prostate Conditions
There are three main conditions every man should know about when it comes to the prostate:
1. Benign Prostatic Hyperplasia (BPH)
BPH refers to the non-cancerous enlargement of the prostate gland, a condition that becomes increasingly common with age. By age 60, about 50% of men will experience symptoms of BPH; by 85, that number rises to 90%.
Common symptoms include:
- Frequent urination, especially at night
- Difficulty starting or stopping urination
- Weak or interrupted urine stream
- A feeling of incomplete bladder emptying
While BPH is not life-threatening, it can significantly affect quality of life and may lead to bladder or kidney issues if left untreated.
2. Prostatitis
Prostatitis is inflammation of the prostate, often caused by bacterial infection, though it can also occur without infection. It can affect men of all ages but is most common in those between 30 and 50.
Symptoms may include:
- Painful urination or ejaculation
- Pelvic or lower back pain
- Urinary urgency
- Flu-like symptoms in acute cases
Treatment depends on the cause but may include antibiotics, anti-inflammatory medications, and lifestyle adjustments.
3. Prostate Cancer
Prostate cancer is the second most common cancer in men worldwide. Most cases grow slowly, and some never become life-threatening. However, aggressive forms can spread quickly, making early detection essential.
Risk factors include:
- Age (risk increases after 50)
- Family history of prostate cancer
- African ancestry
- High-fat diet and obesity
Because early-stage prostate cancer often has no symptoms, regular screening is key for early intervention and survival.
When and How to Get Screened
Routine screening is one of the most effective tools for catching prostate issues early—before they cause major complications. While screening recommendations vary depending on individual risk, most guidelines suggest:
- Start discussions by age 50 for average-risk men
- Start by age 45 for higher-risk individuals (African ancestry or family history)
- Start by age 40 if you have more than one close relative who had prostate cancer early
The two most common screening tools are:
- PSA Blood Test (Prostate-Specific Antigen): Measures the level of PSA in your blood. Elevated levels may indicate prostate enlargement, inflammation, or cancer.
- Digital Rectal Exam (DRE): A physical exam where a healthcare provider checks the size and texture of the prostate.
Neither test is perfect. PSA levels can be elevated for reasons other than cancer, and DREs are limited in scope. But together, they help build a clearer picture of prostate health. If abnormalities are found, your doctor may recommend further tests such as imaging or biopsy.
Lifestyle Choices That Support Prostate Health
While some risk factors like age and genetics can’t be changed, your daily habits have a powerful influence on prostate health. Preventive care isn’t just about screenings—it’s about how you eat, move, and manage stress.
1. Maintain a Healthy Weight
Obesity has been linked to a higher risk of prostate issues, including aggressive prostate cancer. Carrying excess fat can contribute to hormonal imbalances and chronic inflammation—both of which can affect prostate health.
Focus on gradual, sustainable weight loss through proper nutrition and exercise. Even losing 5–10% of your body weight can reduce health risks.
2. Adopt a Prostate-Friendly Diet
What you eat plays a major role in reducing inflammation and supporting hormonal health.
Beneficial foods include:
- Tomatoes: Rich in lycopene, a powerful antioxidant linked to prostate protection
- Cruciferous vegetables: Broccoli, cabbage, and Brussels sprouts contain compounds that support detoxification
- Fatty fish: Salmon, mackerel, and sardines offer anti-inflammatory omega-3s
- Green tea: Contains catechins that may slow prostate cell growth
- Nuts and seeds: Especially pumpkin seeds, which contain zinc and other prostate-supportive nutrients
Avoid high-fat, processed meats, excess dairy, and fried foods. A Mediterranean-style diet focused on whole foods, healthy fats, and plant-based options is one of the most studied and effective dietary patterns for long-term prostate health.
1. Exercise Regularly
Physical activity improves circulation, reduces inflammation, supports weight control, and may lower the risk of BPH and prostate cancer. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, such as walking, swimming, or biking, along with strength training twice a week.
Pelvic floor exercises, also known as Kegels, can also support urinary control, especially for men dealing with BPH or recovering from prostate procedures.
2. Stay Hydrated—but Smartly
While drinking plenty of water is essential for urinary and prostate health, it’s also important to manage fluid intake around bedtime if frequent nighttime urination is an issue. Cut back on fluids 2–3 hours before sleep, and reduce intake of caffeine and alcohol, both of which can irritate the bladder.
3. Limit Alcohol and Avoid Smoking
Alcohol and tobacco use can increase the risk of prostate complications and interfere with overall immune function. Moderate drinking (if any) and smoking cessation not only benefit your prostate but improve your cardiovascular and mental health as well.
Know Your Numbers and Track Changes
Just as you track your weight, blood pressure, or cholesterol, it’s wise to track your prostate health—especially after age 40. If you’re experiencing symptoms such as frequent urination, discomfort, or changes in sexual function, don’t brush it off.
Keep a simple log of any new or unusual changes and share them with your healthcare provider. Prostate issues often progress slowly, and catching them early—through symptoms or screenings—makes a significant difference.
Managing Symptoms and Daily Discomfort
If you’ve already begun experiencing prostate-related symptoms—like frequent urination, urgency, or discomfort—it’s important to know that relief is possible. While these symptoms can be frustrating, especially at night or during social activities, you don’t need to simply “deal with it.”
Lifestyle Adjustments That Help:
- Timed Voiding: Train your bladder by going to the bathroom at scheduled times (e.g., every 3–4 hours), rather than waiting until it feels urgent. This can reduce accidents and urgency.
- Double Voiding: After urinating, wait 20–30 seconds and try again. This helps empty the bladder more fully, reducing the number of trips.
- Avoid Irritants: Caffeine, spicy foods, alcohol, and acidic foods (like citrus) may irritate the bladder and worsen symptoms.
- Elevate Your Legs: If swelling in the legs contributes to nighttime urination, try elevating them an hour or two before bed to reduce fluid retention.
- Bladder Training Exercises: Alongside pelvic floor (Kegel) exercises, strengthening the bladder’s holding capacity can reduce frequency and urgency over time.
These practical strategies, when paired with medical support, can help restore confidence and comfort in everyday life.
Medical Treatments for Prostate Conditions
While lifestyle changes can be very effective, some cases of BPH, prostatitis, or early prostate cancer require medical intervention. Fortunately, today’s treatment options are more varied, effective, and minimally invasive than ever before.
For BPH (Benign Prostatic Hyperplasia):
- Medications:
- Alpha-blockers (e.g., tamsulosin) relax prostate muscles and ease urinary flow.
- 5-alpha-reductase inhibitors (e.g., finasteride) shrink the prostate over time.
- Combination therapies are common and may offer faster relief.
- Minimally Invasive Procedures:
- UroLift System: Lifts and holds the prostate tissue away from the urethra without cutting or removing tissue.
- Rezūm Water Vapor Therapy: Uses steam to destroy excess prostate tissue.
- Surgical Options:
- TURP (Transurethral Resection of the Prostate): A traditional but effective surgery for severe BPH.
Each option has different risks and benefits. A urologist will tailor treatment based on symptom severity, prostate size, age, and lifestyle goals.
For Prostatitis:
Treatment depends on the type:
- Bacterial prostatitis often requires antibiotics, sometimes for several weeks.
- Chronic prostatitis/chronic pelvic pain syndrome may require a combination of anti-inflammatories, pelvic therapy, stress management, and dietary changes.
Relief from prostatitis can take time and patience, but most men improve with the right plan.
For Prostate Cancer:
Treatment varies based on cancer stage and aggressiveness:
- Active Surveillance: For low-risk cases, regular monitoring may be enough without immediate treatment.
- Surgery: A prostatectomy removes the gland; modern robotic-assisted techniques reduce recovery time and side effects.
- Radiation Therapy: External beam or brachytherapy (internal radiation) target cancer cells.
- Hormone Therapy: Reduces testosterone to slow cancer growth.
- Immunotherapy or Targeted Therapies: Used in more advanced or resistant cases.
The key is early detection, which expands treatment choices and improves outcomes significantly.
The Mental and Emotional Side of Prostate Health
Beyond physical symptoms, prostate issues can affect confidence, intimacy, and self-image. Men may feel embarrassed by frequent urination, nervous about medical exams, or fearful of cancer diagnoses. These emotional reactions are valid—and common.
If prostate problems begin affecting your mental health, here are some steps you can take:
- Talk to a therapist or counselor: Processing concerns with a professional can reduce anxiety and help you manage fear or frustration.
- Join a men’s health or prostate support group: Connecting with others going through similar challenges can normalize your experience and offer helpful tips.
- Speak openly with your partner: Concerns about sexual function or energy are easier to manage when addressed honestly and with support.
- Practice stress-reducing techniques: Meditation, breathwork, or exercise help regulate stress and improve sleep and mood.
Mental wellness is deeply tied to physical health. Don’t ignore the psychological impact of prostate-related challenges.
Talking to Your Doctor Without Shame
Many men hesitate to speak with a healthcare provider about prostate symptoms—whether due to embarrassment, fear of bad news, or unfamiliarity with the exams. But open, honest conversations are essential for good care.
Tips for Talking to Your Doctor:
- Write down symptoms before the appointment, including frequency, severity, and any patterns.
- Don’t downplay discomfort. Doctors can only help with what you tell them.
- Ask questions: “What are my treatment options?” “What are the side effects?” “Do I need a specialist?”
- Bring a partner or friend if it makes you feel more comfortable or helps you remember information.
- Follow through on recommended tests—even if you feel fine. Screening is about prevention, not punishment.
Remember: doctors are trained professionals who have these conversations all the time. There is no shame in prioritizing your health.
Busting Myths About Prostate Health
There are plenty of myths and half-truths floating around about prostate health. Here’s what you need to know:
- Myth: Only older men get prostate issues.
Fact: Prostatitis often affects younger men, and BPH can begin in your 40s. - Myth: If I have no symptoms, I don’t need screening.
Fact: Prostate cancer often has no early symptoms. Regular screening helps detect it early. - Myth: Prostate exams are painful or humiliating.
Fact: A digital rectal exam is quick and usually painless. It’s over in seconds—and could save your life. - Myth: Prostate issues always mean cancer.
Fact: The majority of prostate problems are benign. Enlarged prostate and prostatitis are far more common than cancer. - Myth: Treatment always leads to sexual dysfunction.
Fact: Many treatment options preserve sexual function, especially with early intervention and proper planning.
Education is power. When you replace fear with knowledge, you gain control over your health journey.
Prostate Health Across the Decades
Here’s a simple overview of what to focus on as you age:
- In your 30s–40s:
- Learn about prostate health
- Eat a prostate-friendly diet
- Begin regular exercise and stress management
- Talk to your doctor if you have pelvic discomfort or urination changes
- In your 50s:
- Begin or maintain regular screenings (PSA + DRE)
- Monitor changes in urination, energy, and sexual health
- Stay consistent with healthy habits
- In your 60s and beyond:
- Continue regular screenings based on risk
- Monitor for BPH symptoms or prostate cancer signs
- Prioritize comfort, quality of life, and support systems
No matter your age, it’s never too late—or too early—to invest in your prostate health.
Final Word
Prostate health isn’t just a medical issue—it’s a key component of living fully and aging well. With knowledge, attention, and proactive care, most men can prevent or manage prostate conditions before they become serious.
Whether you’re managing symptoms, thinking about screening, or just learning where to start, the most important step is simply this: pay attention and take action. Your body will thank you.
You’re not alone. Millions of men are navigating the same concerns—and with the right information, support, and attitude, prostate health can become part of your strength, not your silence.